In Focus
Dec 19, 2023
Infectious Diseases are not a Sickness but a Social Problem: The deep relationship between infectious diseases and humankind as recounted in history
Infections from the new coronavirus, a highly communicable and dangerous disease that has killed millions, have shocked the world in the past few years. Since the first case was discovered, a deadly battle against this infectious disease has been waged all over the world. Now, more than 3 years later, the sense of fear and anxiety has eased considerably. Humanity has been hit by infectious disease crises many times before and has always been able to keep them under control. What has the fight against infectious diseases taught us? We asked Professor Yasutoshi Kido, a specialist in the field from the OMU Graduate School of Medicine.
The concept of disease has changed dramatically since modern medicine overcame infectious diseases
The list of infectious diseases is a long one: smallpox—traces of which have been found in Egyptian mummies, perhaps ancient victims of what is said to be the oldest recorded infectious disease—cholera, plague, Spanish flu, syphilis, tuberculosis, HIV, SARS, new strains of influenza… even the most well-known culprits alone have taken the lives of countless people. The Black Death killed one third of the population of medieval Europe, and the Spanish flu is estimated to have killed 20 or 40 million people worldwide.
A great many people died of infectious diseases in the past, even when such diseases were not recognized as pandemics, such as the Spanish flu. Until the first half of the 20th century, pneumonia and gastroenteritis were the most common causes of death among people around the world, and these were actually mostly caused by infectious diseases.
“Looking back at human history in terms of average life expectancy, the life span of Homo sapiens when the species first entered the scene was around 30 years, jumping to around 40 years in the 19th century,” explained Professor Kido. “For a long time, human life expectancy did not increase much until about the last 100 years or so, during which it has more than doubled in affluent countries. Behind this is the development of modern medicine. The discovery of the causes of infectious diseases and their cures has contributed greatly to the increase in human longevity.”
Among the people who played a major role in overcoming infectious diseases, Professor Kido focuses on Dr. Robert Koch, a bacteriologist active from the end of the 19th century to the beginning of the 20th century. Dr. Koch discovered Mycobacterium tuberculosis and Mycobacterium cholerae, among others, earning him a nickname as the father of microbiology.
Professor Kido elucidated, “What is amazing about Dr. Koch is that he was the first to say, germs ‘could cause a specific disease,’ as in a germ theory of diseases. Then Dr. Koch showed that microorganisms could be proven to be pathogenic if the three following principles were in place: (1) find a specific microbe in a diseased person who had a particular infectious disease, (2) isolate that microbe, and (3) reproduce the disease with a culture of the isolated microbe. This seems obvious from today’s perspective, but at the time no one was thinking this way. This is why natural therapy where one relocates to the countryside to breathe clean air in an effort to cure tuberculosis was common. Dr. Koch’s idea was that diseases had causes and could be treated by eliminating these causes, which is the basis of modern medicine.”
Dr. Robert Koch established microbiology and paved the way for overcoming infectious diseases
Thus, the basis for treating infectious diseases was established: finding pathogenic bacteria and using drugs that were harmless to humans to kill these bacteria. Antibiotics produced by molds were used as antimicrobial agents, and from the mid-20th century, many infectious diseases became curable or controllable. From there, the threat to people’s health shifted dramatically from infectious diseases to non-communicable diseases such as cerebrovascular disease, cardiovascular disease, and cancer.
“The concept of disease has changed,” noted Professor Kido. “Lifestyle-related diseases are caused by internal changes in the body that result in illness. Various factors influence these diseases, and since there is no identifiable pathogen like with infectious disease, they are diagnosed as a disease if they deviate from the normal population. High blood pressure, obesity, high blood sugar, and lipid abnormalities are now considered ‘diseases’ after their connection to high morbidity rates of heart and brain vascular disease was understood, but the reality is they are more ‘risks’ of becoming diseases’ than diseases.”
Individuals have very different views on how they perceive risk. The Hollywood actress Angelina Jolie’s decision to have a preventive mastectomy because of her risk of hereditary breast cancer is a prime example. After the conquest of infectious diseases, individuals at different periods of time and in different regions have come to vary in their definition of disease.
After a long history together, humans are now in an age when infectious diseases are more likely to occur
According to Professor Kido, there are many traces of the battle against infectious diseases in our bodies. Human beings, like other organisms, have evolved over a long time in directions that most favor producing offspring; many of these evolutions are closely related to infectious diseases. One such example is the relationship between sickle cell disease and malaria. Sickle cell disease is a genetic disorder that causes severe anemia due to a sickle-shaped deformation of red blood cells. In times without medical care, the number of patients with the disease would normally have decreased because they often did not live long enough to produce offspring. However, today there is a high rate of patients in Africa, about 10% in some areas, and this is because sickle cell disease makes people less susceptible to malaria.
“Despite the handicap of severe anemia, some people survived malaria as children and were able to produce more offspring, and their genes are still being passed on today,” Professor Kido continued. “This is just one example, but I think it is fair to say that inscribed in our genes is a triumphant history of human beings enduring deadly infectious diseases to stand the test of time.”
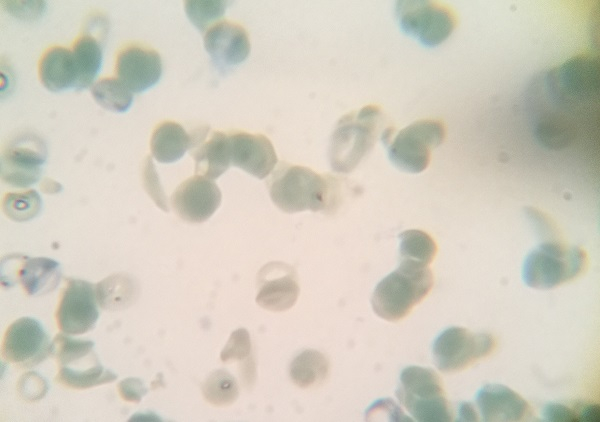
Caption: Normal red blood cells are disc-shaped, but sickle cell disease causes sickle-shaped (crescent-shaped) red blood cells to appear
Humanity has a history of constantly battling new infectious diseases, and it can be said that humans and pathogens have evolved in a perfect balance for each to survive.
“New pathogens don’t suddenly appear from nothing; they originate from something on Earth,” insisted Professor Kido. “They may have been limited to some regions or in the bodies of organisms, or they may have been trapped in thick ice at some point, but they are there. It is important to note that this is now changing dramatically.”
Infectious diseases are caused by a complex interplay of three factors: agent, host, and environment. Professor Kido stated that “in the past 20 years alone, the number of new infectious diseases has increased, the new coronavirus being one of them,” pointing out further that of the three factors, the host and environment have changed significantly.
“Climate change and the progress of development cause shifts in the ecosystem, increasing contact between infected animal species and humans and thereby increasing the chance of humans also becoming a host species for pathogens. In addition, as globalization progresses and people and goods move around the world, contact with new infectious diseases will also increase. In this sense, we are living in an era in which new infectious diseases are more likely to occur.”

Caption: Professor Kido discussing the diverse relationships between infectious diseases and humankind
The fight against infectious diseases is not just a medical problem. How do we build a society that is resistant to infectious diseases?
If development and globalization are inextricably linked to the emergence of new infectious diseases, it is highly likely that new diseases will appear again in the future. How should we deal with them?
Professor Kido emphasized that the problem of infectious diseases is a “social problem.” It is important to establish a comprehensive philosophy on how to handle them as a society, and then take full measures in accordance with that philosophy.
“In the early days of COVID-19, the declaration of a state of emergency required restrictions on outings, travel, schools, restaurants, events, and other economic activities. While these restrictions were intended to protect the constitutional human right to health, they also led to restrictions on the right to liberty, which is also guaranteed by the constitution. The question of how far to go in restricting the right to liberty is an extremely serious one. When infectious diseases arise, the world tends to become anxious and restrict or monitor the behavior of others. The important thing is not to eliminate those who are infected, but rather to become more tolerant of infection and create a society that is kind to those not feeling well.”
Professor Kido said that one problem, for example, is the state of the healthcare system. “Restrictions on hospital visits occurred in Japan during COVID-19, limiting people’s access to medical care. Japan’s universal health insurance system is supposed to have the advantage of allowing people to see a doctor anytime as long as they pay a certain amount of premiums, but during the outbreak many people were unable to see a doctor or were forced to receive medical treatment at home. The main reason for this was the difference between what was required of hospitals during normal times and during COVID-19. Normally, hospitals are required to operate at a high level of efficiency in Japan, with no empty beds allowed, but suddenly they were asked to provide many beds, and there was a limit to how much they could do.”
Professor Kido said that allowing the diagnosis and treatment of healthy people with no symptoms at pharmacies is one way to improve access to care and reduce the burden on medical institutions. In any case, it is necessary for those of us who pay insurance premiums to take an interest ourselves and think carefully about what should be done with the healthcare system in the future.
“In order to face infectious diseases, both society and the individual must be robust—have the strength to be less susceptible to infectious diseases—and resilient—have the ability to recover from severe impacts. The key to building this is the trust and solidarity of community. Infectious diseases are not a problem that can be tackled only with medicine. I think it is important for everyone to understand how to balance health and freedom, and to think about what kind of society will not be defeated by infectious diseases.”
Researcher’s details

Professor Yasutoshi Kido
Department of Basic Medical Science, Graduate School of Medicine, Osaka Metropolitan University. Current position since 2022.
PhD (Health Sciences), Physician.
Graduated from the Faculty of Science and Engineering, Waseda University, and from the Faculty of Medicine, Oita University; completed a doctoral course at the Graduate School of Medicine and Faculty of Medicine, The University of Tokyo.
His main areas of research are microbiology, molecular epidemiology, and clinical pharmacology in the field of emerging and reemerging infectious diseases. He has studied global infectious diseases such as the three major infectious diseases of TB, AIDS, and malaria in Africa, neglected tropical diseases, and new coronavirus infections.
SDGs

